Common Indications for CRRT in ICU Patients

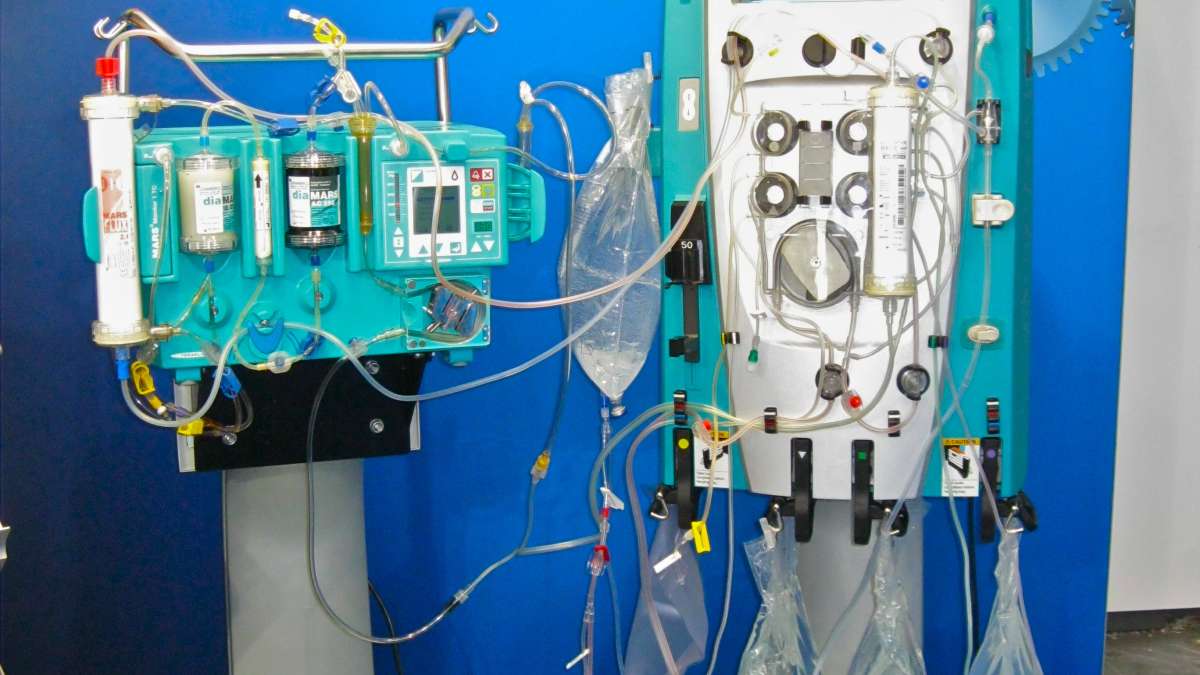
Continuous Renal Replacement Therapy (CRRT) is a life-saving intervention used in the Intensive Care Unit (ICU) for patients with acute kidney injury (AKI) and other critical conditions requiring continuous kidney support. Unlike traditional intermittent hemodialysis, CRRT provides slow and continuous removal of waste products, electrolytes, and fluids, making it an ideal therapy for hemodynamically unstable patients. In this article, we will explore the most common indications for CRRT in ICU patients and the clinical scenarios where it is most beneficial.
1. Acute Kidney Injury (AKI)
One of the primary indications for CRRT is Acute Kidney Injury (AKI), particularly in critically ill patients who cannot tolerate conventional hemodialysis. AKI is characterized by a sudden decline in kidney function, leading to an accumulation of waste products and electrolyte imbalances. Common causes of AKI in ICU patients include:
- Sepsis: A systemic infection that can cause multi-organ failure, including the kidneys.
- Hypotension and Shock: Decreased blood flow to the kidneys can lead to ischemic injury.
- Nephrotoxic Medications: Drugs such as aminoglycosides, contrast agents, and NSAIDs can induce kidney damage.
- Rhabdomyolysis: Breakdown of muscle tissue releases myoglobin, which is toxic to the kidneys.
- Multi-Organ Dysfunction Syndrome (MODS): Kidney failure as part of widespread organ failure.
CRRT is preferred over intermittent hemodialysis in these cases because it provides gentler and more controlled fluid and solute removal, reducing the risk of further hemodynamic instability.
2. Fluid Overload and Refractory Edema
Critically ill patients, especially those with cardiac dysfunction, sepsis, or massive fluid resuscitation, are prone to fluid overload. Excess fluid can lead to:
- Pulmonary Edema: Fluid accumulation in the lungs, impairing oxygen exchange.
- Worsening Cardiac Function: Increased preload and afterload can strain a failing heart.
- Tissue Hypoxia: Impaired oxygen delivery due to excessive interstitial fluid.
CRRT allows for gradual and precise fluid removal, preventing sudden intravascular volume shifts that could worsen hemodynamic instability.
3. Severe Electrolyte Imbalances
Critically ill patients often develop life-threatening electrolyte disturbances that necessitate CRRT. These include:
- Hyperkalemia (Severe Potassium Elevation): A critical condition that can cause life-threatening cardiac arrhythmias.
- Severe Metabolic Acidosis: A common issue in AKI, sepsis, and shock states.
- Hyperphosphatemia: Common in kidney failure and can contribute to further metabolic derangements.
- Hyponatremia or Hypernatremia: Rapid correction of sodium imbalances is dangerous, and CRRT provides a controlled method to manage these levels gradually.
CRRT is especially useful when rapid or large shifts in electrolyte levels could cause neurological or cardiovascular instability.
4. Sepsis and Septic Shock
Sepsis is one of the most common reasons ICU patients require CRRT. In severe cases, sepsis leads to:
- Cytokine Storm and Inflammatory Response: Excessive inflammatory mediators contribute to multi-organ failure.
- Acute Kidney Injury: Secondary to hypotension, inflammatory damage, and microvascular thrombosis.
- Metabolic Dysregulation: Sepsis often causes profound acid-base and electrolyte disturbances.
CRRT not only manages fluid and electrolyte imbalances but may also help in removing inflammatory mediators, reducing the severity of the cytokine storm in some patients.
5. Drug and Toxin Removal
CRRT is used in ICU patients to facilitate the removal of drugs and toxins, particularly in cases of overdose or poisoning where the kidneys cannot effectively eliminate the substance. Common situations include:
- Drug Overdose: Lithium, salicylates, methanol, ethylene glycol, and other dialyzable toxins.
- Severe Lactic Acidosis: Due to metformin toxicity or mitochondrial dysfunction.
- Tumor Lysis Syndrome (TLS): Occurs in cancer patients undergoing chemotherapy, leading to massive electrolyte disturbances and kidney failure.
CRRT provides continuous and controlled clearance of these toxins while maintaining hemodynamic stability.
6. Liver Failure and Hepatorenal Syndrome
Patients with severe liver disease or hepatorenal syndrome (HRS) often develop profound metabolic imbalances, fluid overload, and AKI. CRRT is beneficial in these cases for:
- Correcting Acidosis and Electrolyte Imbalances
- Managing Volume Overload
- Supporting Kidney Function Until Liver Transplantation or Recovery
For patients awaiting liver transplantation, CRRT can be a bridge therapy to maintain stability.
7. Pediatric and Neonatal Critical Care
CRRT is increasingly used in pediatric and neonatal ICUs for managing acute kidney injury, congenital heart disease, and metabolic disorders. Its gradual and continuous nature makes it safer for neonates and infants who cannot tolerate rapid fluid and solute shifts.
CRRT is a vital tool in the management of critically ill ICU patients with acute kidney injury, fluid overload, severe electrolyte disturbances, sepsis, drug toxicity, liver failure, and cardiorenal syndrome. Unlike traditional dialysis, CRRT provides continuous and hemodynamically stable therapy, making it the preferred option for unstable patients. As advancements in technology continue to refine CRRT techniques, its role in critical care will only expand, improving outcomes for some of the sickest patients in the ICU.